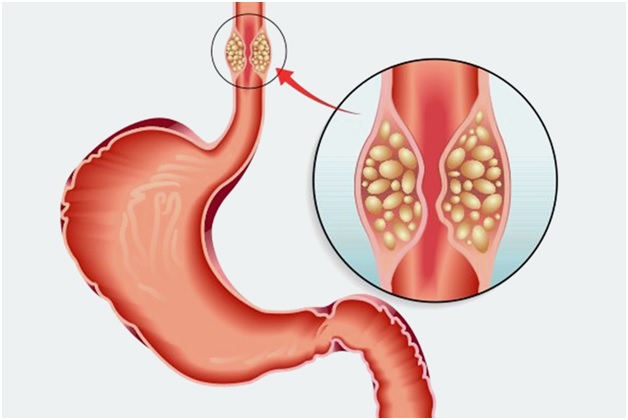
Oesophageal cancer is a serious condition affecting the food pipe, causing difficulty in swallowing and impacting overall health. Over time, treatment approaches have advanced significantly, with radiation therapy becoming increasingly precise and patient-focused. Modern developments aim to improve effectiveness while reducing side effects, making care safer and more comfortable for patients.
Radiation therapy is commonly used alongside surgery or chemotherapy, depending on the stage and health of the patient. In centres offering esophagus cancer treatment in Delhi, modern radiation techniques help target tumours accurately while minimising exposure to healthy tissues. These innovations have transformed the way doctors plan and deliver therapy, supporting better outcomes and patient experience.
Understanding Radiation Therapy in Oesophageal Cancer
Radiation therapy uses high-energy beams to target cancer cells and limit their growth. In oesophageal cancer, it is often part of a structured treatment plan. It may be given before surgery to reduce tumour size, after surgery to address remaining cancer cells, or as the main treatment when surgery is not suitable. Radiation is also used to relieve symptoms such as difficulty swallowing or chest discomfort, helping improve daily comfort.
Earlier techniques affected larger areas of the chest, sometimes impacting nearby organs. Modern planning and imaging now allow doctors to focus radiation more precisely on the tumour, reducing exposure to healthy tissue. Recent advancements continue to improve accuracy, comfort, and overall treatment experience.
Modern Advances in Radiation Therapy for Oesophageal Cancer
Recent developments in radiation therapy have improved accuracy, reduced complications, and enhanced patient comfort. The following advanced techniques are now widely used in clinical practice.
Image-Guided Radiation Therapy (IGRT)
Image-Guided Radiation Therapy (IGRT) uses frequent imaging during the treatment course to confirm the tumour’s position. Since the oesophagus moves slightly due to breathing or swallowing, IGRT ensures radiation is delivered precisely to the target. This reduces unnecessary exposure to surrounding organs and maintains consistent treatment accuracy throughout the treatment.
Intensity-Modulated Radiation Therapy (IMRT)
Intensity-Modulated Radiation Therapy allows clinicians to adjust the intensity of radiation beams across different parts of the tumour. Higher doses can target cancer cells, while lower doses can affect nearby healthy tissues. IMRT has been shown to reduce side effects such as oesophageal inflammation and lung irritation, improving patient tolerance and reducing interruptions during therapy.
Volumetric Modulated Arc Therapy (VMAT)
VMAT is an advanced form of IMRT in which radiation is delivered as the machine rotates around the patient. This method helps in shorter treatment sessions while maintaining precise dose delivery. Shorter sessions improve patient comfort and are especially helpful for those who find it difficult to remain still during treatment.
Proton Beam Therapy
Proton beam therapy is an emerging option in selected cases of oesophageal cancer. Unlike conventional radiation, protons release most of their energy directly at the tumour site, minimising exposure to nearby healthy organs such as the heart and lungs. While not yet widely available in India, this technique represents an important area of ongoing research.
Adaptive Radiation Planning
Adaptive radiation therapy allows the treatment plan to be modified during therapy based on changes in tumour size or patient anatomy. This approach ensures radiation remains accurate throughout the treatment period and reflects a more responsive, patient-specific method of care.
Managing Side Effects with Modern Techniques
Radiation therapy can sometimes cause side effects, but modern techniques focus on minimising these complications. Care teams monitor patients closely to ensure that treatment is both safe and tolerable. The following approaches help manage common issues:
- Swallowing discomfort: Soft or liquid diets can ease difficulty during treatment.
- Fatigue: Patients are encouraged to balance rest with light activity to maintain energy.
- Skin irritation: Gentle skin care with mild moisturisers prevents irritation in exposed areas.
- Nutritional support: Regular assessments by nutrition specialists help patients maintain adequate strength and weight.
- Symptom reporting: Promptly informing the care team of new or worsening symptoms allows timely adjustments to the treatment plan.
These measures, combined with precise radiation techniques, help patients complete therapy with fewer interruptions and a better overall experience.
Role of Multidisciplinary Care
Radiation therapy is most effective when delivered as part of a coordinated plan involving a multidisciplinary team. Oncologists, radiologists, surgeons, and supportive care specialists work together to determine the best approach for each patient. Access to advanced imaging and experienced clinical teams ensures accurate diagnosis and precise treatment planning, resulting in safer, more effective therapy.
Conclusion
Advances in radiation therapy have significantly improved care for people with oesophageal cancer. Techniques such as IGRT, IMRT, VMAT, proton therapy, and adaptive planning allow for more precise targeting, fewer side effects, and greater patient comfort. Multidisciplinary care and patient-specific planning are essential to maximise the benefits of these innovations.
These developments make modern radiation therapy a key component of oesophagus cancer treatment in Delhi, offering patients more effective and compassionate care. Early diagnosis, accurate treatment planning, and supportive care remain critical to achieving the best possible outcomes.