Vasectomy is a widely accepted surgical procedure used for permanent male contraception. While considered safe and minimally invasive, vasectomy has been under scrutiny for potential systemic and organ-specific effects beyond the reproductive tract. Among the most debated is its possible relationship with prostatic inflammation and chronic pelvic disorders. This article explores the hypothesis that vasectomy contributes to the alteration of prostatic inflammatory pathways through complex immunological, hormonal, and structural mechanisms.
Understanding Vasectomy: A Brief Overview
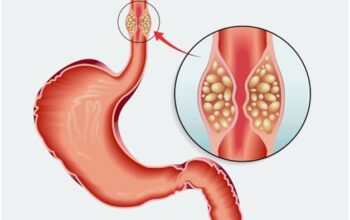
Vasectomy involves the surgical occlusion or severance of the vas deferens, the ducts that carry sperm from the testicles to the urethra. It is typically performed under local anesthesia, and complications are rare. However, a percentage of individuals develop post-vasectomy pain syndrome (PVPS), which may involve pelvic discomfort, testicular pain, and in some cases, prostatitis-like symptoms. This has prompted researchers to investigate the deeper connections between vasectomy and prostatic inflammatory pathways.
Prostatic Inflammation: Mechanisms and Mediators
The prostate gland is a critical component of the male reproductive system, producing seminal fluid and modulating sperm motility. Inflammatory processes within the prostate are categorized as:
- Acute bacterial prostatitis
- Chronic bacterial prostatitis
- Chronic pelvic pain syndrome (CPPS)
- Asymptomatic inflammatory prostatitis
Regardless of the subtype, these conditions are marked by elevated levels of cytokines, such as IL-6, TNF-α, and IL-8, infiltration of immune cells, and increased oxidative stress. The possible intersection of vasectomy with these immune and inflammatory pathways has become a compelling area of investigation.
Hypothesized Links Between Vasectomy and Prostatic Inflammation
1. Sperm Antigen Exposure and Autoimmune Activation
One of the most plausible mechanisms linking vasectomy to prostatic inflammation is the exposure of sperm antigens to the immune system. Normally, sperm are protected within the blood-testis barrier, a highly specialized barrier that maintains immune privilege. Following vasectomy, sperm may leak into surrounding tissues due to increased intraluminal pressure, triggering autoimmune responses.
These immune responses are not necessarily confined to the site of leakage. Through molecular mimicry and systemic immune activation, the prostate gland may also become a target of T-cell-mediated inflammation, particularly when sperm-specific antigens resemble prostatic proteins.
2. Backpressure Effects on the Epididymis and Prostate
Post-vasectomy, increased luminal pressure in the vas deferens and epididymis can lead to secondary effects on nearby structures, including the prostate. Studies have demonstrated ductal dilation, epithelial damage, and interstitial fibrosis in animal models, which may contribute to neurogenic inflammation and activation of afferent pain pathways involving the pelvic plexus. Chronic stimulation of these pathways may amplify prostatic inflammatory signaling.
Vasectomy, Immune Surveillance, and Chronic Prostatitis
The immune landscape of the prostate is tightly regulated. Following vasectomy, this balance may be disrupted through several processes:
- Elevated systemic immune activity leads to increased recruitment of neutrophils and macrophages to the prostate.
- Altered lymphatic drainage due to local scarring and fibrosis changes the cytokine milieu.
- Increased oxidative stress post-vasectomy can prime the prostate for chronic inflammation and tissue remodeling.
Histological analyses in some animal studies have shown infiltrative immune cells in the peri-prostatic region after vasectomy, supporting the idea that the procedure may trigger low-grade, chronic immune responses that culminate in inflammation.
Endocrine Crosstalk: Hormonal Imbalance and Prostatic Sensitivity
Another potential pathway linking vasectomy to prostatic inflammation involves subtle changes in androgen metabolism. Though serum testosterone levels generally remain unchanged, local androgen receptor signaling in prostatic tissue may be modified due to altered feedback mechanisms between the testicles and accessory sex glands.
Androgens, particularly dihydrotestosterone (DHT), are essential for maintaining prostate health. Dysregulation of androgenic control can predispose the prostate to inflammatory insults and may modify epithelial permeability, immune cell behavior, and stromal responsiveness.
Clinical Evidence: What Do Studies Say?
The data linking vasectomy to prostatic inflammation are still evolving. Some epidemiological studies have suggested a weak association between vasectomy and prostatitis-like symptoms, while others have found no significant correlation. However, recent advances in biomarker analysis and molecular imaging have begun to identify subtle inflammatory changes in post-vasectomy patients:
- Increased expression of IL-1β and IL-6 in seminal plasma post-vasectomy.
- Elevated leukocyte counts in expressed prostatic secretions.
- MRI evidence of structural remodeling in peri-prostatic tissues.
Despite these findings, the overall clinical risk remains low. Most vasectomy patients do not experience persistent prostatitis or chronic pelvic symptoms, underscoring the multifactorial nature of such conditions.
Animal Studies and Experimental Models
Preclinical models have provided some of the strongest evidence for the vasectomy-prostate inflammation hypothesis. In rodent models, vasectomy has been associated with:
- Disruption of epithelial junctions in the prostate.
- Increased infiltration of mast cells and macrophages.
- Higher rates of stromal fibrosis and epithelial metaplasia.
Interestingly, these changes are often time-dependent, appearing weeks or months after the procedure. This supports the idea that vasectomy-induced inflammation is a delayed, progressive process rather than an immediate postoperative event.
Vasectomy, Inflammation, and Prostate Cancer: A Controversial Link
Another debated area is the possible association between vasectomy and prostate cancer. Some studies have reported a modest increase in prostate cancer risk in men who underwent vasectomy, possibly due to chronic inflammation as a carcinogenic factor. Inflammatory cytokines can promote DNA damage, angiogenesis, and epithelial-mesenchymal transition, all of which are implicated in tumor progression.
However, meta-analyses and large cohort studies have largely refuted a strong causal link. While chronic inflammation may play a role in carcinogenesis, the evidence does not currently support vasectomy as a significant risk factor for prostate cancer.
Future Directions: Biomarkers and Personalized Screening
As research continues, the identification of biomarkers for post-vasectomy inflammation may help stratify risk in susceptible individuals. Potential markers under investigation include:
- Pro-inflammatory cytokines (IL-6, IL-8, TNF-α)
- Matrix metalloproteinases (MMPs)
- Seminal oxidative stress markers
- Prostatic stromal cell gene signatures
Additionally, advancements in non-invasive imaging and functional urodynamics could improve diagnosis and monitoring of post-vasectomy prostatic health.
Should This Impact Vasectomy Counseling?
Despite the emerging data, vasectomy remains a highly effective, low-risk method of permanent birth control. However, informed consent should evolve to reflect our growing understanding of long-term outcomes. Men considering vasectomy should be counseled about rare but possible post-procedural inflammatory sequelae, including symptoms consistent with chronic prostatitis or chronic pelvic pain syndrome.
For men with a preexisting history of prostatitis or pelvic pain, urologists may consider further evaluation before proceeding with vasectomy.
Conclusion
The intersection between vasectomy and prostatic inflammatory pathways reflects a complex biological interplay involving immune activation, structural changes, and hormonal modulation. While the majority of vasectomy patients experience no long-term issues, a small subset may develop prostatitis-like symptoms due to these multifactorial effects. Continued research is needed to clarify causality, identify at-risk individuals, and refine treatment approaches for post-vasectomy inflammatory syndromes.
FAQs
1. Can vasectomy cause chronic prostatitis?
Vasectomy does not directly cause chronic prostatitis in most men. However, some may experience inflammatory responses or pelvic pain that mimic prostatitis symptoms. These responses are likely immune-mediated and occur in a minority of patients.
2. Is there a link between vasectomy and prostate cancer?
The majority of large-scale studies have found no strong evidence that vasectomy increases the risk of prostate cancer. Early studies suggesting a link may have been confounded by detection bias and other variables.
3. How is post-vasectomy inflammation treated if it occurs?
Treatment for inflammation potentially associated with vasectomy includes NSAIDs, alpha-blockers, pelvic floor physical therapy, and in rare cases, vasectomy reversal or denervation procedures. Management depends on the severity and persistence of symptoms.